Early Uses of Cancer Vaccines
The immune system is amazing. It adapts to the environment the organism finds itself in. Components of the system are able to distinguish between cells that are supposed to be in the body and intruders or diseased cells. This includes malignant cancer cells, which the immune system can attack. Many micro-tumors are kept from exploding into clinical cancers through vigilance of the immune system. Healthy cells are not attacked except in situations of auto-immune diseases. Cancer often manipulates the immune system and makes it apply the same controls to malignant cells it applies to healthy cells. Immunotherapy more or less erases the cancer illusion. When it works, it kicks the immune system back into action and allows it to attack the cancer.
A vaccine that prevents cancer by preventing infection by the human papilloma virus (HPV), the cause of nearly all cases of cervical cancer, has already been approved by the FDA. The new drug is called Gardasil and was 100% effective in preventing HPV infection in a trial of 9,000 women. Although Gardasil only works against the two strains of HPV that cause 70% of cervical cancers, it could still save the lives of 210,000 women per year if administered widely.
 Gardasil is made from purified, inactivated proteins from the HPV virus, which serve as the antigens that mount the immune response, and vaccination consists of 3 shots over eight months. Because it is a vaccine against the virus, not against the cancer cells themselves, it prevents all symptoms of HPV infection, including genital warts.
Gardasil is made from purified, inactivated proteins from the HPV virus, which serve as the antigens that mount the immune response, and vaccination consists of 3 shots over eight months. Because it is a vaccine against the virus, not against the cancer cells themselves, it prevents all symptoms of HPV infection, including genital warts.
Cervical cancer is the second-leading cause of cancer death among women, killing 300,000 each year. About 10% of these deaths occur in the United States, while the majority occur in Latin America and Africa. HPV infection is still rampant in the United States, with about 6.2 million Americans becoming infected every year and the majority of American men and women becoming infected at some point in their lifetime. The low death rate in the United States is due to the relative ease of detecting cervical cancers early with regular Pap smears (a gynecological examination in which part of the cervical tissue is scraped off and examined for signs of cancer). If it were not for this early diagnosis, the United States would suffer a death rate similar to Africa’s or Central America’s, and poor Americans without access to healthcare are already in such a situation. Thus, Gardasil has the potential to alleviate the death rate in the third world while substantially diminishing healthcare costs in the United States.
Wider vaccination against the hepatitis B virus would also have drastic effects on the worldwide cancer rate. Those infected with hepatitis B experience a 20- to 100-fold increase in their risk of liver cancer, and half of all liver cancers test positive for hepatitis B. The vaccine would be especially useful to the people of sub-Saharan Africa and Southeast Asia, where the virus is most prevalent. Although the vaccine has already been developed, its use is not widespread.
There is substantial potential to decrease the risk of stomach cancer by fighting infection as well. The Epstein-Barr virus is known to cause stomach cancer, and researchers are in the process of developing a vaccine against it. Heliobacter pylori is a bacterium that infects the stomachs of about half of the people on Earth and has recently been linked to a four- to six-fold increase in the risk of stomach cancer.
There is a good chance that active specific immunotherapy is likely to become part of a multimodal approach to cancer. Patients will be treated with chemotherapy and surgery in addition to vaccines. The medical profession must get a better understanding of adjuvants administered with tumor cell vaccines.
Four types
(1) tumor immune cell-based vaccines, (2) peptide-based vaccines, (3) viral vector-based vaccines, and (4) nucleic acid-based vaccines (especially mRNA vaccines).
Oncophage
The world’s first therapeutic cancer vaccine, Oncophage, was approved in Russia in 2008 for the treatment of kidney cancer. The United States FDA did not approve it at that time because it found that the trials conducted by the American developer Antigenics showed insufficient proof of a significant benefit. Since then, the FDA has granted fast-track and orphan drug status to Oncophage and trials are currently being conducted for the treatment of kidney cancer, metastatic melanoma, and glioma, a form of brain cancer.
Oncophage is produced using actual cells from the patient’s tumor to create a specific agent to fight only the targeted cancer. In this way, healthy tissue is left unharmed and the drastic side effects of other therapies like chemotherapy are largely eliminated.
Prostvac and Provenge
Provenge (Sipuleucel-T) has also been approved for prostate cancer.
Prostvac (rilimogene galvacirepvec/rilimogene glafolivec), another vaccine being developed to treat metastatic prostate cancer, has been fast-tracked by the FDA and is undergoing large-scale clinical trials. In previous trials, it has demonstrated a median overall survival improvement of 8.5 months, but like sipuleucel-T, does not meet the criteria for non-progressive survival.
Prostvac, unlike sipuleucel-T, is not patient-specific. It uses two viruses along with other know immune system stimulators. The first virus is vaccinia-PSA-TRICOM, which is injected once to ready the immune system for a response to the cancer. The second, fowlpox-PSA-TRICOM, is administered multiple times for continual boosting of the immune system.
Antigens
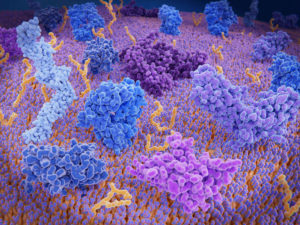
Human cells are enclosed in membranes and the outsides of the membranes often have ligands attached that function as antigens in the immune systems. Among other functions, the antigens identify the cell as part of the body. Cells with the wrong antigens are considered as foreign invaders by the immune system. The A/B/AB/O blood types derive from the antigens on red blood cells. O type cells do not have antigens that activate the immune system, which is why O type blood can be given to anyone with little fear of a negative reaction. A type blood has antigens that make it acceptable for people with A blood, but which produces an immune response in people with O or B blood.
Other webpages:
https://www.cancer.gov/news-events/cancer-currents-blog/2019/in-situ-vaccine-non-hodgkin-lymphoma
https://www.cancer.gov/news-events/cancer-currents-blog/2017/melanoma-personalized-vaccine
https://www.cancerresearch.org/en-us/immunotherapy/treatment-types/cancer-vaccines
https://www.nature.com/articles/nri.2017.140
https://pubmed.ncbi.nlm.nih.gov/33907315/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3721379/
 Today’s arsenal of chemotherapy agents includes many different classes of medicines. Researchers continue to find and test new drugs.
Today’s arsenal of chemotherapy agents includes many different classes of medicines. Researchers continue to find and test new drugs.