Kinase Inhibitor Drugs
Kinase inhibitors are now one of the major categories of chemotherapy medicine. Over 50 kinase inhibitors are approved in the US for cancer treatment with more under development. Of the 69 new drugs approved by the FDA for cancer from 2015 to 2020, 26 were kinase inhibitors. This is one of the most active areas of medical chemistry research.
Protein enzymes are chains of amino acids and when a phosphoryl group, PO32−, is covalently attached to one of the amino acids, it changes the three-dimensional configuration and function of the protein. Proteins are constantly being phosphorylated and dephosphorylated in living cells. Apoptosis, proliferation, and differentiation are all affected by phosphorylation. Kinases are a class of enzyme that promote phosphorylation. When these kinases go wrong, normal cellular function can go awry. Kinase deregulation can contribute to the growth of cancer.
Drugs given to stop kinases can slow the proliferation of malignant cells and angiogenesis (growth of blood vessels). There are many kinases (over 500 in the human body). They play overlapping and intricate roles in tumor initiation, survival and proliferation. Many kinase inhibitor compounds have been found. Some of these have proved to be useful in cancer treatment.
Most kinase inhibitors work on tyrosine kinases. These enzymes promote transfer of a gamma phosphate group from ATP to a tyrosine residue on a protein. This chemical reaction functions as a signal transduction mechanism. Other kinases work on serine or threonine residues. Like tyrosine, serine and threonine are amino acid building blocks for protein. As oncology drugs, kinase inhibitors were created out of modern genetics- the understanding of DNA, the cell cycle, and molecular signaling pathways- and thus represent a change from general to molecular methods of cancer treatment. This allows for targeted treatment of specific cancers, which lessens the risk of damage to healthy cells and increases treatment success.
The first kinase inhibitor introduced for cancer was imatinib, which the FDA approved in 2001. An article published in the journal Molecular Cancer in 2018 claimed that over 10,000 patents had been filed in the US for kinase inhibitors since 2001. Scientists are looking the possibility of kinase inhibition for other diseases including hypertension and Parkinson’s disease but here we focus on cancer medicines.
Tyrosine kinase inhibitors
Tyrosine kinase inhibitors (TKIs) are a class of chemotherapy medications that inhibit, or block, one or more of the enzyme tyrosine kinases. Cell membrane receptors are what scientists call molecular structures that send and receive signals from the environment. Some of the receptors are enzymes and catalyze biochemical reactions.
Receptor Tyrosine Kinases (RTKs) are a family of tyrosine protein kinases. RTKs span the cell membrane with an intracellular (internal) and extracellular (external) portion. The intracellular portion removes a phosphate group, a process called dephosphorylation, from the coenzyme messenger ATP. The extracellular portion has sites to which signal sending proteins and hormones can bind. Many of these signaling binders are growth factors.
Growth factors are involved in the initialization and regulation of cell cycles. The type of growth factor determines its effects on the cell. There are three primary growth factors that relate to tyrosine kinase. The receptors of these growth factors are members of the RTK family. Epidermal growth factors (EGF) help regulate cell growth and differentiation. Platelet-derived growth factors (PDGF) regulates cell growth and development. Vascular endothelial growth factors (VEGFR) are involved in the creation of blood vessels.
The growth factors, and the kinases, act together as though they are attached to an “on/off” switch. The removal of a phosphate group changes the shape and actions of the protein. This essentially “turns on” the cellular action (or actions). When the cellular action(s) is completed, the phosphate group is removed and that protein is “turned off.” This “on/off” process can become disrupted, often by a mutated kinase, and actions can become unregulated. An unregulated RTK bound to EGF, for example, could lead to uncontrolled growth and division in the cell. The rapid cell growth could then lead to cancer. Mutations of RTKs often lead to oncogenes, which are genes that help turn a healthy cell into a cancerous cell.
Tyrosine kinase inhibitors treat cancer by correcting this deregulation. Imatinib, for example, blocks a kinase receptor from binding to ATP, preventing the phosphorylation that would benefit the cancerous cell and promote cell division. Gefitinib inhibits epidermal growth factor receptors (EGFRs), preventing those signals from being stuck “on” and creating uncontrolled proliferation.
Over 30 TKI medications, including imatinib and gefitinib, have been approved by the Food and Drug Administration for use in humans. One TKI, Toceranib (Palladia), was approved 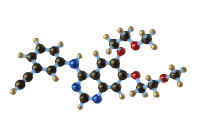 for the treatment of cancer in dogs. The medications may inhibit one or more tyrosine kinases. Erlotinib (Tarceva), like Gefitinib, inhibits EGFR. Lapatinib (Tykerb) is a dual inhibitor of EGFR and a subclass called Human EGFR type 2. EGFR isn’t the only growth factor targeted. Sunitinib (Sutent) is multi-targeted, inhibiting PDGFR and VEGF.
for the treatment of cancer in dogs. The medications may inhibit one or more tyrosine kinases. Erlotinib (Tarceva), like Gefitinib, inhibits EGFR. Lapatinib (Tykerb) is a dual inhibitor of EGFR and a subclass called Human EGFR type 2. EGFR isn’t the only growth factor targeted. Sunitinib (Sutent) is multi-targeted, inhibiting PDGFR and VEGF.
Other tyrosine kinase inhibitors are more specialized. Sorafenib (Nexavar) targets a complex pathway that would lead to a kinase signaling cascade. Nilotinib (Tasinga) inhibits the fusion protein bcr-abl and is typically prescribed when a patient has shown resistance to imatinib.
More TKIs are currently in development, though the process is slow and more drugs end up being abandoned during clinical phases than get approved.
ALK inhibitors
ALK stands for anaplastic lymphoma kinase. The first ALK inhibitor, crizotinib, is now considered the first-generation of drugs in this class. Crizotinib works on ALK and also on the pathways ROS1 and MET. In early tests scientists found this medicine inhibited the ALK pathway and that this pathway might be a good target for anti-cancer drugs. Some (not all) patients with non-small cell lung cancer have a mutation in the ALK gene system.
The second generation of ALK inhibitors include ceritinib, alectinib, and brigatinib. Other drugs are in development and lorlatinib was given orphan drug status by the FDA, The drugs work on cells that have “chromosomal rearrangements” of ALK.
These are a form of personalized therapy. The doctor can order a test of the biopsy tissue removed from the cancer. If it indicates the malignant cells have the ALK mutation (are said to be ALK-positive), these inhibitors are thought to be a good potential form of treatment.
BTK Inhibitors
Bruton’s tyrosine kinase (BTK) is critical in development of certain blood cells (mast cells and B cells). Three drugs that inhibit this protein have been approved for cancer therapy:
FLT3 inhibitors
Cats can get a cancer called Feline McDonough Sarcoma and it was when studying this that scientists identified an oncogene – which occurs in humans too – that is associated with dysregulation of a type of receptor tyrosine kinase. This fms-like tyrosine kinase 3 (FLT3) plays a key role in creation of new blood cells and hence is of interest to researchers looking into leukemia. Compounds called FLT3 inhibitors have been developed. Like other tyrosine kinase inhibitors they attach to the ATP binding site of the kinase and prevent phosphorylation of the protein.
Only three FLT3 inhibitors are on the market. Midostaurin is approved for acute myeloid leukemia, but the label says the AML should be FLT3-positive. In other words, an analysis of the malignant blood cells should show a mutation of the FLT3 gene. But that’s still a big number of potential patients because 30 percent of AML cases test positive for this mutation. Gilteritinib was approved in 2018, also for leukemia, and Pacritinib was approved in 2022 for myleofibrosis.
The FLT inhibitor Quizartinib is used in Japan, but not approved in the US. Crenolanib is another second generation FLT3 inhibitor under investigation.
Sorafenib also shows some inhibition of FLT3 although we are not including it in this class for the purposes of this website.
JAK Inhibitors
Janus Kinases are one form of tyrosine kinase. When discovered they were given the name JAK for “just another kinase”, but these were later renamed for the Roman god Janus. Several drugs have been developed to block JAK; only two, Ruxolitinib and Pacritinib, are used for cancer patients.
Serine and threonine kinase inhibitors
Serine and threonine kinases target serine and threonine residues on the DNA, and there are medicines that inhibit those enzymes, too. Some targets that medicinal chemists go after include MAP kinases, ERK, stress-activated JNK, and p38 kinases. An interesting subclass is aurora kinases which are important in cell reproduction (they are central to mitosis and meiosis.) Aurora kinases are overexpressed in some forms of cancer, especially leukemia, and several dozen drugs in development target them.
BRAF inhibitors
BRAF is a gene that encodes creation of some growth factor enzymes – the enzymes are part of the system that tells cells how to differentiate, where to go, and when to die. If the BRAF gene mutates, it can result in cancer. (BRAF is an “oncogene”.) Scientists estimate 5 to 10 percent of human cancers involve a mutated BRAF gene. BRAF mutations appear to be present in half of melanoma and papillary thyroid cancers, 3 percent of lung adenocarcinomas, and 10 percent of colorectal cancers. They also occur in leukemia and brain cancers. BRAF is part of the mitogen-activated pathway (MAP) group of kinases.
Medicines classified as BRAF inhibitors – or B-Raf inhibitors – affect enzymes made by the mutated BRAF gene. Analysis of the biopsy tissue can tell whether a case has this mutation. If so, that cancer is a candidate for BRAF inhibitor treatment. Patients who are given BRAF inhibitors usually get an MEK inhibitor also.
Sorafenib – considered both a BRAF inhibitor and a tyrosine kinase inhibitor
Regorafenib – considered both a BRAF inhibitor and a tyrosine kinase inhibitor
Cyclin-dependent kinase inhibitors
Cyclin-dependent kinases are another type of proteins involved in the cell cycle. There are 21 enzymes in this class and they are named sequentially – CDK-1, CDK-2, etc.
Compounds that inhibit these enzymes are under investigation for use as cancer treatments. Some medicines are specific in targeting certain enzymes, e.g. CDK-4 inhibitor, while others are considered multi-CDK inhibitors.
When a cell starts to reproduce, it is CDK4 and CDK6 that are part of the biochemical cascade that starts that cycle. CDKs are also involved in the transition from the G1 to M phase (CDK-2) and the G2 to S phase.(CDK-1).
Scientists have developed over 30 CDK inhibitors; this is one of the hottest areas in medicinal chemistry. They are being investigated for treatment of cancer and other diseases including Cushing Disease and cystic fibrosis. Three CD4/6 inhibitors have been approved for treatment of breast cancer.
Abemaciclib (Verzenio) inhibits CDK-4 and CDK-6
Palbociclib (Ibrance) inhibits CDK-4 and CDK-6
Ribociclib (Kisqali) inhibits CDK-4 and CDK-6
Other Kinase Inhibitors
MEK inhibitors
One class of enzymes is the oddly named mitogen-activated protein kinase kinase (the double use of “kinase” is not a mistake, these are referred to as MAP2K, MEK, MAPKK.) These catalyze phosphorylation of mitogen-activated protein kinase (MAPK). The MAPK pathway is a chain of reactions that transmit signals from the surface of the cell to the nucleus, and is important in how the body determines what proteins to make and when cells should divide. The MAPK pathway is “dysregulated” in an estimated 50 percent of human cancers. Scientists have developed drugs to inhibit these enzymes, and hence to slow the multiplication of malignant cells.
Tropomyosin kinase inhibitors
Only one tropomyosin kinase inhibitor has been approved by the FDA: Larotrectinib. Mutations in the genes for this kinase are more often found in relatively rare cancers, but one estimate is that 5000 diagnosed cases a year harbor tropomyosin receptor kinase fusions.
Breakdown of Types of Kinase Inhibitors
Advantages of Kinase Inhibitors
Scientists are interested in kinase inhibitors because they more precisely go after cancer cells than older chemotherapy medicines did. All chemotherapy drugs seek to stop cell division and growth. An inherent weakness in cancerous cells is that a failure of mechanisms to repair damaged or changed DNA effectively.
Destruction of healthy cells is one of the main problems with traditional chemo treatments. Kinase inhibitors, however, are targeted and act upon pathways that have gone awry in the specific cancer. This specificity results in fewer side effects and less time in the hospital for the patient. In many cases it is feasible to screen tumor biopsies to see if a particular patient’s cancer has a mutation that can be targeted by the drug.
Today kinase inhibitors are often used as part of a combination chemotherapy regimen, but observers hope that clinicians will eventually be able to use kinase inhibitors without conventional chemotherapy drugs. Because malignant cells grow quickly and consume a good amount of energy, scientists looked into whether intermittent fasting by the patient could control cancer growth. Some scientific work shows that fasting plus administration of kinase inhibitors may be as effective as conventional chemotherapy without as severe side effects.
According to an article published in late 2018, kinase inhibitors account for one-fourth of the pharmaceutical industry’s research and development efforts.
Covalent Kinase Inhibitors
Medicinal chemists designate some medicines as “covalent drugs” which bind to target proteins in a tight bond. These drugs have been around for a long time for many diseases, although they have tended to be discovered by serendipity, not through rational drug development. Some kinase inhibitors fit into the covalent category. These include EGFR inhibitors, KRAS inhibitors, and ErbB inhibitors.
Oral Administration
Many kinase inhibitors are taken orally. Oral administration opens up the possibility for a potential glitch in the dose sizing as pharmacodynamic models are built on the assumption of certain uptake rates in the patient’s digestive system. If the patient takes an antacid or proton pump inhibitor the adsorption of the kinase inhibitor in the intestines could be reduced. Further, if the patient or caregiver breaks the pill before swallowing it, the rate of adsorption could be higher than the pharmacodynamic model assumes. For some drugs this won’t matter, but the pills are formulated with the assumption they will be swallowed whole.
 Today’s arsenal of chemotherapy agents includes many different classes of medicines. Researchers continue to find and test new drugs.
Today’s arsenal of chemotherapy agents includes many different classes of medicines. Researchers continue to find and test new drugs.