Paclitaxel
One of the most widely used chemotherapy agents
Paclitaxel is an anti-cancer drug, also known as Taxol and Onxol. The drug is first-line treatment for ovarian, breast, lung, and colon cancer and second-line treatment for AIDS-related Kaposi’s sarcoma. It is so effective that some oncologists refer to the period before 1994 as the “pre-Taxol” era for treating breast cancer.
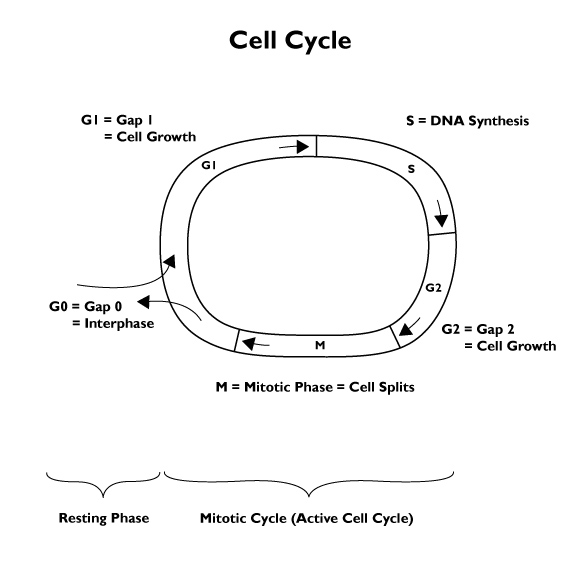
Paclitaxel is classified as an antimicrotubule agent; it stops the growth of the cancer by inhibiting multiplication of malignant cells. During mitosis, the cell uses structures called microtubules to move around the chromosomes. This class of chemotherapy drug works by throwing a wrench into the G2-Phase and M-Phase of the cell cycle.
Taxol is typically administered intravenously. (Oral administration has been demonstrated but is rarely used.) It is supplied as a clear, viscous, non-aqueous concentrate, in 30mg/5 ml to 30mg/50ml multi dose vials. The diluted solution is stable at ambient temperatures and room lighting conditions for 24 hours. Normal IV tubing and filters are employed.
The drug goes throughout the body (“systemic”) and gets in all tissues and fluids, which can lead to negative side effects. For some cancers, oncologists put the Taxol in a bodily cavity to concentrate its effect in one part of the body.
A common regimen would be 175 mg / m2 delivered over 3 hours every 3 weeks for 4 cycles in combination with another chemotherapy agent. Severe hypersensitivity reactions occur in 2-4% of patients. (Fatal reactions have occurred but are rare.)
Related to paclitaxel is docetaxel. Both are grouped in the taxane chemotherapy drug class. Docetaxel (taxorene) is made from a chemical extracted from the leaves of the European yew tree, Taxus baccata. This source is more plentiful and renewable than the Pacific Yew bark that paclitaxel was originally derived from, and the high cost and scarcity of paclitaxel in the early days was a spur to research that led to docetaxel.
A Bioprospecting Success Story
Paclitaxel is one of the most recognizable, celebrated, and controversial products in the fight against cancer. Some have called paclitaxel a miracle drug. Since doctors started using it for the treatment of breast cancer, the survival rate has doubled. (This increase in survival rate is not all due to the paclitaxel.) Paclitaxel as a commercial product has received the ire of conservationists, holds records for sales volume, and has been the subject of public debate and congressional hearings. Its discovery and development as a drug is a fascinating story of chance, intuition, expensive risk taking, perseverance, and success.
After a study of medicinal herbs and folkloric knowledge, extracts from juniper trees were found to have some anti-cancer properties. This led to a search for more active conifers. In 1962, a botanist working for the US Department of Agriculture in Washington State was sampling trees with “cancer plant” potential. The 1645th plant sample collected was a Pacific Yew tree. This tree is a very slow growing hardwood that grows in the shadows of giant conifers and has long been considered a “trash tree”. The tree has very few pests because almost every part of the tree is poisonous. Historically, the wood from the Yew tree has been good for making bows as well as poison arrows; it is associated with death. The Latin name Taxus brevifolia is related to the word “toxin”.
The FDA approved paclitaxel for cancer treatment in 1992. In addition to the brand name Taxol, Paclitaxel is sold in Canada under the names Abraxane® and Apo-Paclitaxel®. In Mexico it goes by the names Aclixel, Asotax, Bristaxol, Cryoxet, and Praxel .
Pacitaxel Treatment
Paclitaxel is given as a shot to the vein (intravenously). A licensed physician supervises administration, although a nurse or technician often sticks the tube into the blood vessel. It takes a while for the drug to enter the circulatory system, so the patient is hooked up for over 30 minutes. The time for treatment varies considerably for different patients and different cancers. Sometimes it takes hours to administer the Paclitaxel.
It is common for patients to be “premedicated” with dexamethasone. This is a steroid that acts as an anti-inflammatory and can help stop the patient from getting nauseous during administration of the Paclitaxel.
Because Paclitaxel is a toxin, healthcare providers use gloves. Topical exposures have resulted in tingling, burning and redness.
The website uptodate.com reports these typical dosages
Ovarian carcinoma:
I.V.: 135-175 mg/m2 over 3 hours every 3 weeks or
135 mg/m2 over 24 hours every 3 weeks or
50-80 mg/m2 over 1-3 hours weekly or
1.4-4 mg/m2/day continuous infusion for 14 days every 4 weeks
Oncologists use their experience and judgement to set the regimen. Intraperitoneal (unlabeled route): 60 mg/m2 on day 8 of a 21-day treatment cycle for 6 cycles, in combination with I.V. paclitaxel and intraperitoneal cisplatin. Note: Administration of intraperitoneal paclitaxel should include the standard paclitaxel premedication regimen.
According to an article in the International Journal of Women’s Health, “no ideal dosing strategy for paclitaxel exists in ovarian cancer”. Attempts to establish an ideal regimen have produced mixed results.
Metastatic breast cancer:
I.V.: 175-250 mg/m2 over 3 hours every 3 weeks or
50-80 mg/m2 weekly or
1.4-4 mg/m2/day continuous infusion for 14 days every 4 weeks
Nonsmall cell lung carcinoma:
I.V.: 135 mg/m2 over 24 hours every 3 weeks
AIDS-related Kaposi’s sarcoma:
I.V.: 135 mg/m2 over 3 hours every 3 weeks
or 100 mg/m2 over 3 hours every 2 weeks
Early clinical trials resulted in unprecedented success in treating ovarian cancer. Taxol had become a miracle drug. The sudden demand for Yew bark led to illegal “Taxus Rustling” and a legal cottage industry harvesting the trees. These new jobs were seen locally as replacements to the declining timber industry. It was obvious to everyone that the demand was unsustainable. Although chemists figured out how to do laboratory synthesis of Paclitaxel, it was not practical. A process that involves biotechnology (plant cell fermentation) is now used to produce the world’s supply of Taxol. By 1995, all dependence upon the Pacific Yew was eliminated.
The popularity of this effective drug made it a blockbuster. Bristol Myers Squibb reported sales of their branded product, Taxol, were almost $1.6 billion in 2000. There were numerous patents for various applications, which began to run out in the late 1990’s. A generic version of the Taxol formulation, Onxol, came on the market in 2000.
Administration
Paclitaxel is administered as part of a liquid solution. It’s dissolved in polyoxyethylated castor oil (often a branded solvent called Kolliphor EL – formerly Cremophor) and ethanol. Strictly speaking, Taxol refers to the solution rather than the Paclitaxel itself. The side effects of Paclitaxel, like those of many agents, are due to systemic administration – the drug travels  through the bloodstream to the whole body and it stops fast-multiplying cells in the hair follicles and intestines (resulting in hair loss and nausea.)
through the bloodstream to the whole body and it stops fast-multiplying cells in the hair follicles and intestines (resulting in hair loss and nausea.)
Patients taking anticonvulsant medicines can tolerate a higher dosage of Paclitaxel. If you take phenytoin or phenobarbital your liver might be better able to eliminate the toxic chemotherapy drug.
Taxol has another downside that other chemotherapy agents don’t have in that the Kolliphor and ethanol are toxic. It also does not work well with a range of other medicines. Consult your healthcare provider before starting any new medicine, including over-the-counter products. Make sure your supervising doctor know all drugs you are taking.
Innovators are trying to improve chemotherapy delivery with materials science. Small spheres with paclitaxel enclosed are one viable option researchers are looking at. More on delivery.
Elimination
Paclitaxel exits the body mostly through the feces. Less than 20% comes out in the urine. Some is broken down by the liver. For a 3-hour administration, the half-life is under 24 hours. For a 24-hour infusion, the half-life is a couple days.
Side Effects of Paclitaxel
Most Paclitaxel patients lose their hair – it usually grows back – and experience some nausea or vomiting. Patients are also at increased risk of infection because your immune system is compromised. Chemotherapy drugs tend to have dose-limiting toxicity in one organ system. For Paclitaxel that system is the bone marrow, and myelosuppression, a weakening of the immune system, is common. Indeed, the most common side effect appears to be lowering of blood cell counts.
A diagnostic test called the absolute neutrophil count is given to patients, and generally those with a white blood cell count below 1500 cells/mm^3 (before any chemo treatment) are not given Paclitaxel. When patients in the course of a treatment get severe neutropenia (neutrophil <500 cells/mm3) it is common for the treating oncologist to lower the dosage by about 20%. Doctors also check to ensure that the platelet count is >=100,000 cells/mm3.
Cancer results in uncontrolled growth of malignant cells in the body. These cells are destroyed by Paclitaxel and other anticancer drugs that prevent them from multiplying rapidly. However, normal healthy cells may also get damaged and side effects are usually a result of damage done to these cells. Cells more susceptible to damage are the fast-growing normal cells that include blood cells present in the bone marrow and cells present in the mouth, stomach, intestines, and esophagus that together make up the digestive tract. Since hair follicles can also be affected, hair loss may occur during chemotherapy.
Common side effects include
- hair loss (scientific name: alopecia)
- nausea and vomiting
- diarrhea
- mouth sores
- low blood cell count (either red cells or white cells or both)
Less common but more serious side effects are
- chest pain
- irregular heartbeat (bradycardia)
- usual bleeding or bruising
- hypotension (low blood pressure
- numbness and pain in hands (peripheral neuropathy)
If your Paclitaxel affects your lungs, heart, kidneys, bladder and nervous system, let your doctor know right away. Also inform your doctor about unusual bleeding or numbness or tingling in fingers or toes.
Paclitaxel patients (both male and female) should use contraception if there is any chance of pregnancy. Tests in animals show Paclitaxel harms embryos, fetuses, and expecting mothers. It is never given to pregnant women. Breast-feeding women are never given Paclitaxel.
Interactions with other Chemotherapy Drugs
Paclitaxel is often given as part of a combination chemotherapy regimen. Oncologists have to weigh many factors in determining the best regimen and the potential interactions between drugs. The monoclonal antibody trastuzumab seems to have more severe cardiovascular side effects when combined with Paclitaxel. Topotecan, etoposide, and doxorubicin are all known to increase the chances of adverse reactions when taken with Paclitaxel. The widely used chemotherapy drug Cisplatin – when taken with Paclitaxel the negative effect on white blood cell count is more pronounced. The timing of the delivery of these drugs is important.
Background of this medicine
When early drug developers were trying to get an effective drug from the Yew tree, separating the chemical fractions from the bark samples was a difficult and slow process. It required skill and intuition by the researchers, using equipment that can now be found only in museums.
Research on the extracted chemicals was arduous and nearly every chemical turned out to be so toxic to humans that it killed every cell, not just cancerous ones. One promising compound needed a name long before its structure was determined. They simply named it from the source, “Taxus” with the ending for alcohol, “ol” without any real consideration. “Taxol” was found to have already been trademarked in the 1930’s by a French company for a laxative product. However, the drug company Bristol Myers Squibb was able to purchase the trademark and convince the Patent and Trademark office that a common laxative trademark should now apply to an anticancer drug.
Research was very slow. Supply was a challenge because the Yew tree was rare and grew very slowly. Paclitaxel solubility in water was described by one researcher as being equivalent to that of brick dust. It was not clear that Taxol could be administered to patients. Severe hypersensitivity in some clinical patients and failures as an anti-leukemic drug nearly stopped research on this chemical.
By 1971 scientists had established that Taxol displayed some promise as an anticancer agent. However, there was great reluctance to even harvest enough for clinical trials. The Pacific Yew tree is not common. Each tree could supply about 2 kilograms of bark. 12 kilograms of bark was needed to produce one half gram of Taxol. The Yew tree dies after stripping the bark.
In 1977, an order for 7,000 pounds of bark was made. This meant killing 1,500 trees, scattered in patches over millions of acres of old growth forests in the Pacific Northwest. This coincided with and became enmeshed in the debate over the spotted owl habitat. The need for natural remedies and medicinal herbs conflicted with conservationists and brought considerable notoriety to Taxol.

Ground-up Yew Tree Bark, in days when paclitaxel was made from bark.
Public domain Source: Mike Trumball, Hauser Northwest
Paclitaxel was found to promote regression of mammary tumors in 1978. The next year, it was found that the Paclitaxel mechanism was unique. Older anti-cancer compounds killed cancer cells by inhibiting the production of the building blocks that are needed for the cell to divide. Paclitaxel stimulates the production of the building blocks such that the cells cannot coordinate cell division. In the cell division cycle, it works in the G2 (Gap 2) and M phases, by stabilizing microtubules and inhibiting their disassembly. This essentially stops cell reproduction, and slows the growth of cancer. When the drug gets inside the reproducing cell, it can distort mitotic spindles, causing chromosomes to break.
In 1992 the US government passed the Pacific Yew Act to ensure “that Federal lands will be managed to provide for the sustainable harvest and long-term conservation of the Pacific yew.” In 1984 Congress’s Waxman-Hatch Act (among other things) gave Bristol Myers Squibb exclusive marketing rights to Taxol for five years.
The drug showed great success in cases of metastatic breast cancer. In 1992 the FDA approved the drug and Bristol-Myers Squib put it on the market at a wholesale price of just under $1000 for each dose. (Patients typically got 4 or 5 doses per year.) At the time, it was the most expensive drug on the market, although compared to some of today’s drugs, it was relatively cheap.
Who knows – there may be numerous anti-cancer agents yet to be discovered from plant, marine, and fungal sources. Cancer is not a single disease. It is several hundred diseases and will almost certainly require many agents for treatment. The Taxol story shows the utility of searching for highly active natural products. It was a successful business venture as well as a medical success, saving many lives.
Note: In 2011 the International Union for Conservation of Nature designated a species of Asian Yew Tree used to harvest paclitaxel as endangered.