Vaccines for Cancer Prevention
If vaccination can be used to stop infectious diseases, can it be used to prevent cancer? Some scientists are asking this question. Cancer vaccines can be divided into two categories: therapeutic and preventative. Cancer centers throughout the world are working on creating vaccines in both categories.
Optimists think over 15% of cancer cases could be stopped by fighting infections. The proportion is even larger in the Third World, where an estimated one in four cancers is linked to infection. It is easier, cheaper, and more effective to vaccinate against viruses that lead to cancer than it is to treat the cancer by conventional means or through a cancer treatment vaccine. Prevention is where most of the benefit from cancer vaccines is likely to come from in the near future.
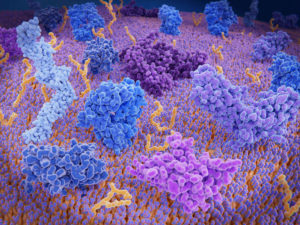
Regardless of which strategies are used to direct the immune response against the tumor or the virus that causes tumors, additives that help boost general immune response are often used. Bacteria, viruses, cytokines (molecules used by the immune system to communicate between cells), as well as various chemicals cause the immune system to increase its response and are therefore often added to vaccines.
The immune system is more effective when it has to fight a smaller number of cells, so cancer vaccines work best when the tumor has already been removed by standard means, such as chemotherapy, radiation, or surgery. When attacking single tumor cells or small clumps of tumor cells, T cells and B cells take care of business, but an entire tumor overwhelms the body’s limited number of T and B cells. With the exception of vaccines against cancer-causing viruses, which will be given to prevent cancer, cancer vaccines show most promise for preventing the resurgence of cancer after the tumor has been removed.
There is also evidence that a universal cancer vaccine may be possible. Researchers from Duke University Medical Center in Durham, North Carolina and Geron Corp. of Menlo Park, California are targeting a protein called telomerase, which is present in all major human cancers. The telomerase vaccine will not be as effective as vaccines made from a patient’s own tumor antigens, but it may be very useful when combined with other universal antigens. So far, the vaccine has been able to stimulate immune cells to slow tumor growth in mice and kill unrelated human cancer cells in the test tube.
Most antigens used in allogenic vaccines are only specific to one type of cancer, and a few are expressed in two or more types. For example, Carcinoembryonic antigen is found on 90 percent of colon cancers and 40 percent of breast cancers but is still absent from most types. Telomerase, however, is required for cells to divide many times, as it elongates the ends of the chromosomes that are chopped off as cells undergo mitosis. Cancer cells have to divide many times rapidly in order for the tumor to grow, so they virtually always express telomerase. Scientists were initially worried that the body would not mount an immune response against telomerase, because non-cancer cells that need to divide continuously (such as the cells that create new sperm) also express telomerase, so the body may not recognize it as foreign.
To stimulate the T and B cells to recognize telomerase as foreign, the team inserted the RNA that codes for telomerase into APC’s (the cells that present antigens to the B and T cells) in order to induce them to display telomerase on their surface. Once the APC’s are displaying telomerase, the T cells and B cells will recognize it as foreign and mount an immune response. The result is a vaccine that is only moderately effective, but is effective with virtually every type of cancer cell. Once other universal cancer antigens are identified, their combined use may produce a broadly effective vaccine.
These promising early-stage studies, however, are often later proved wrong when re-tested with a larger sample size. For example, one early-stage study that indicated that a melanoma vaccine would help to prevent melanoma recurrence was later surpassed by a larger trial of 774 subjects that showed the vaccine to be less effective than the alternate treatment of high-dose interferon.
Availability of Cancer Vaccines
The first monoclonal antibody therapy treatment, approved in 1986, was made from the B cells of mice. Because the antibodies were slightly different than those produced by humans, the immune systems of the patients produced antibodies against the mouse antibodies in 85% of subjects. This made the treatment far less effective, and future antibody treatments focused on human B cells.
 Scientists say the future is promising for cancer vaccines. With the advancements made in cancer treatment vaccines and the demonstrated success of cancer prevention vaccines and monoclonal antibody treatment, it is difficult not to be optimistic. More time will still be needed for cancer treatment vaccines, however, as the immediate benefits lie in the expansion of treatment by and development of vaccines to prevent cancer-causing viruses.
Scientists say the future is promising for cancer vaccines. With the advancements made in cancer treatment vaccines and the demonstrated success of cancer prevention vaccines and monoclonal antibody treatment, it is difficult not to be optimistic. More time will still be needed for cancer treatment vaccines, however, as the immediate benefits lie in the expansion of treatment by and development of vaccines to prevent cancer-causing viruses.
Therapeutic cancer vaccine research and development faces many challenges. An effective cancer vaccine must contain several components, including tumor antigens, immunological adjuvants, delivery systems, and immunosuppression modulators, which need to be chosen in the optimal combination to fight the particular cancer. Many highly complex and coordinated clinical trials are required to determine this combination. Availability of these components can also be an issue, either from a supply standpoint or a confidentiality standpoint. Obtaining the desired components and getting permission to combine them in such ways can be difficult. Furthermore, monitoring of immunological response must be state-of-the-art in order to compare and rank different combinations in order of effectiveness.
To face these challenges, the Cancer Vaccine Collaborative (CVC) was formed. It is a partnership between the Cancer Research Institute and the Ludwig Institute for Cancer Research Ltd., two of the leading cancer immunology research organizations in the world. The organization employs leading immunologists in design of complex clinical trials and immunological response measurement, two keys to development of the best possible vaccines to fight cancer.
Dozens of clinical trials are currently underway to evaluate therapeutic vaccines for treatment of many forms of cancer, including bladder cancer, brain tumors, breast cancer, cervical cancer, Hodgkin’s Disease, kidney cancer, melanoma, multiple myeloma, leukemia, lung cancer, Non-Hodgkin’s Lymphoma, pancreatic cancer, and prostate cancer.
Sources:
https://www.cancer.net/navigating-cancer-care/prevention-and-healthy-living/hpv-and-cancer
https://www.cdc.gov/cancer/prevention/vaccination.html
https://www.cancerresearch.org/en-us/immunotherapy/treatment-types/cancer-vaccines