Dose-Dense Chemotherapy
This is a system – a philosophy – of chemotherapy drug administration. It’s the shock and awe of drug delivery. The idea is to deliver a knockout punch to the cancer. There are many good reasons to give chemo this way. Total treatment time is shorter than under older regimens, and the patient can get off chemo sooner – which given side effects and costs associated with chemo is desirable. The downside is that in the short run the side effects can be more severe.
In a dose-dense regimen, the oncology team delivers a series of infusions with little time between them.
Dose-dense can be used with either monotherapy (single chemo agent) or a combination regimen. It overcomes the resistance of malignant cells and clinicians hope it will beat the remission problem that happens when longer periods are allowed between administrations.
Dose-dense administration is given in all stages of cancer, as first-line treatment, as second-line treatment, and as neoadjuvant treatment. It is less common in adjuvant (post surgery or radiation) treatment and is never used palliatively, Sometimes abbreviated as DDC, this method is also called maximum tolerated dose (MTD).
Dose dense chemo is often applied with simultaneous myeloid growth factors, such as filgrastim (Neupogen) and pegfilgrastim (Neulasta) and sargramostim (Leukine). This is to help the body cope with the assault on blood cell production the high medication doses induce.
Before dose-dense regimens became so prevalent, a widely used standard administration regimen involved giving the patient the medicine with breaks of three or four weeks between doses. This was done in recognition of how harsh the drugs are – the time was to allow for side effects to subside. But this time also allowed small rapidly growing tumors to grow.
Older systems used smaller doses with longer periods between treatment. Does dense uses higher doses and less time between doses. Clinical trials with different types of cancer and different regimens show dose-dense is more effective at eliminating cancer.
Some Math
To understand the idea behind dose-dense therapy, look to the Gompertzian growth model of tumor activity. Why do they call it Gompertzian growth? Benjamin Gompertz did some work in mathematical biology in the 19th Century, with applications for populations of animals. The Gompertz function is a sigmoid function – it describes slow growth early and faster growth as the tumor grows. If there is a limit on resources (e.g. nutrients) there will be a slow-down in growth at some point in time. Tumors can escape this slow-down to some extent by growing their own blood vessels (angiogenesis). But in the earlier stages of tumor growth the Gompertz function has been demonstrated to more or less accurately describe the rate of growth in solid tumors.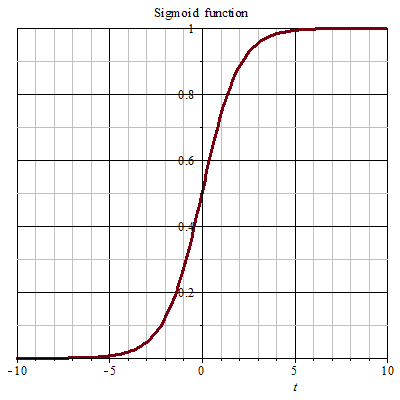
More on mathematical models of cancer growth.
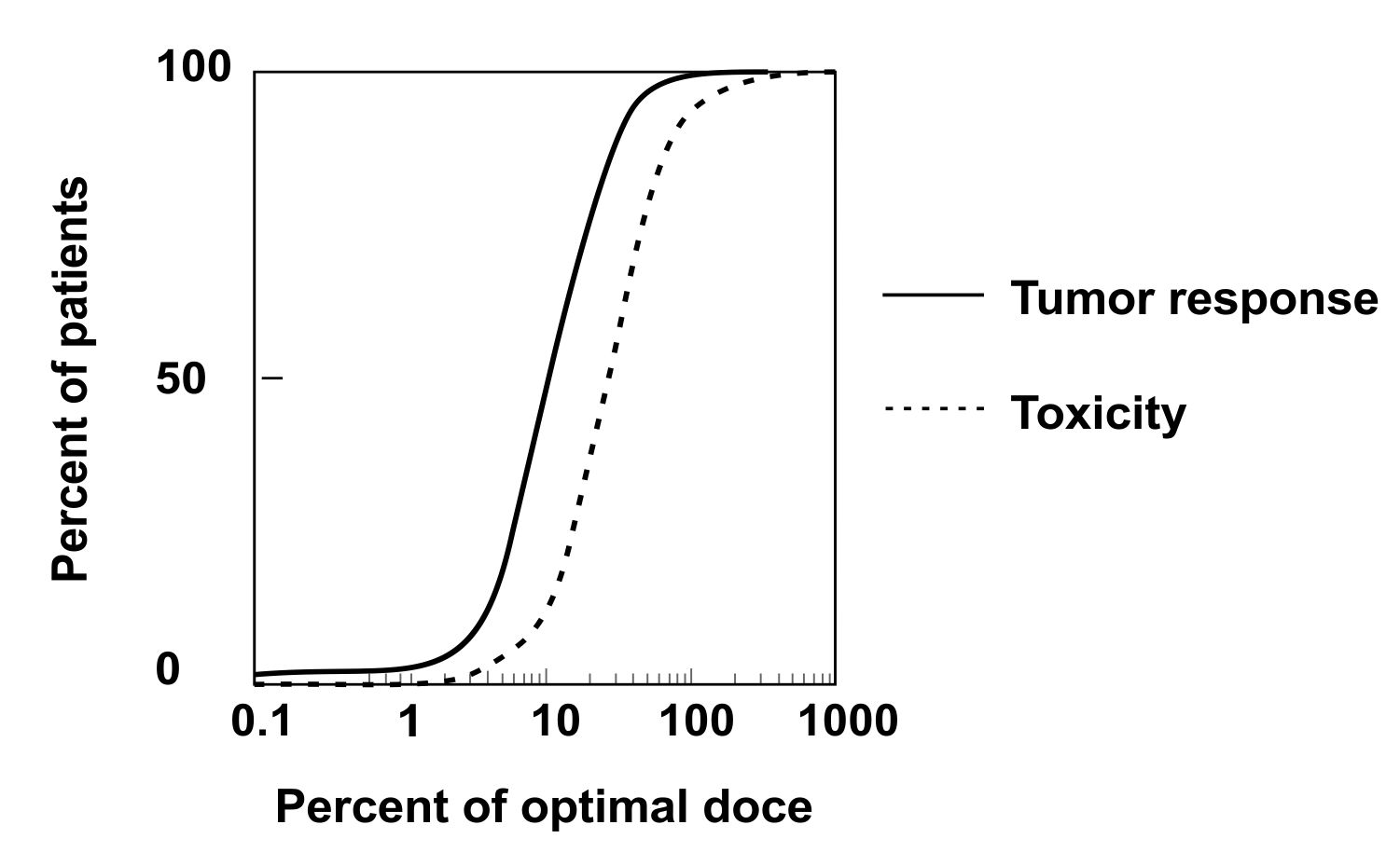
Downsides are side effects and toxicity
The patient might ask: can’t I just start with a little? A low dose to see how it goes? While that might be a good plan for a lot of drugs in other areas of medicine, it’s a bad idea for chemotherapy treatment of cancer because cancer adapts to drugs. The cancer can mutate inside the body and learn to survive in an environment with chemotherapy drugs. The last thing an oncologist wants to do is cultivate resistance – to train the cancer to handle the medicine. To eradicate the cancer, you have to hit it hard and fast and kill it beyond the ability to grow back. That’s why dose-dense administration works.
Studies have shown that dose-dense approaches can have long-term benefits. Patients treated with this approach for one combination of drugs for breast cancer saw higher 10-year survival rates than those treated with a standard regimen, and that improvement was true regardless of HER2 or estrogen-receptor status.
The downside – at least in this breast cancer study – was that patients on the dose-dense more often got leukemia and myelodysplastic syndrome.
Sources: https://pubmed.ncbi.nlm.nih.gov/17370924/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3947590/
https://pubmed.ncbi.nlm.nih.gov/21076605/
https://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-14-515
https://cancerres.aacrjournals.org/content/73/1/119.short
 Today’s arsenal of chemotherapy agents includes many different classes of medicines. Researchers continue to find and test new drugs.
Today’s arsenal of chemotherapy agents includes many different classes of medicines. Researchers continue to find and test new drugs.